Different immune responses identified in patients with COVID-19
The largest study of its type in the UK has identified differences in the immune response to COVID-19 in people with no symptoms, compared to those suffering a more serious reaction to the virus.
Researchers from the Wellcome Sanger Institute, Newcastle University, University College London, the University of Cambridge, EMBL’s European Bioinformatics Institute (EMBL-EBI), and their collaborators within the Human Cell Atlas initiative found raised levels of specific immune cells in asymptomatic people infected with SARS-CoV-2. They also showed that people with more serious symptoms had lost these protective cell types, but had increased numbers of inflammatory cells.
Insights from single-cell sequencing
The research, published in Nature Medicine, is one of the only studies to date that has included people who were asymptomatic. This large-scale collaborative study is part of the Human Cell Atlas initiative to map every cell type in the human body, to transform our understanding of health, infection, and disease.
To understand how different immune cells responded to the infection, researchers analysed blood from 130 people with COVID-19. These patients came from three different UK cities – Newcastle, Cambridge, and London – and their conditions ranged from asymptomatic to critically severe.
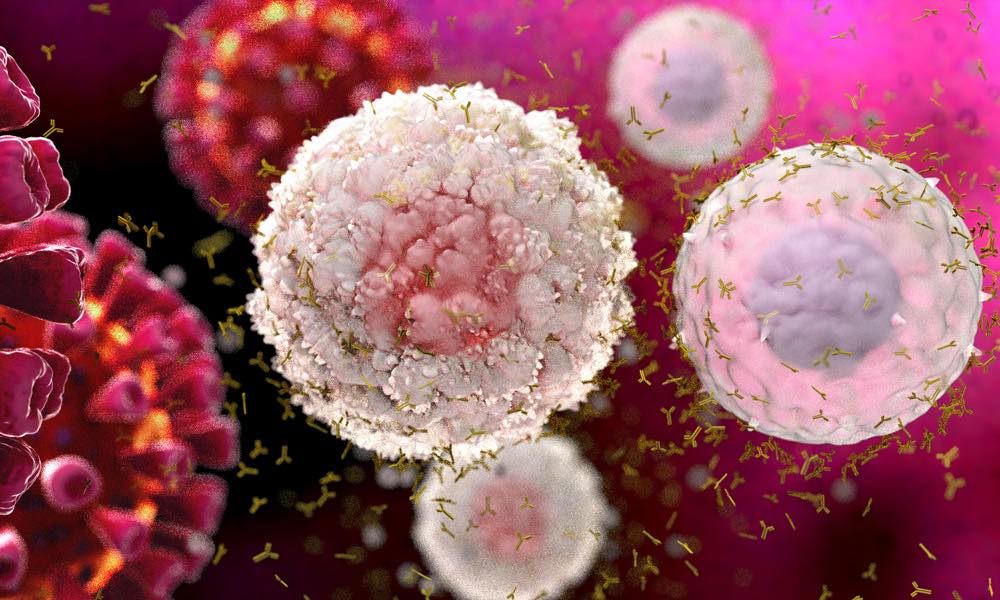
The team performed single-cell sequencing on approximately 800,000 individual immune cells, along with detailed analysis of cell surface proteins and antigen receptors found on immune cells in the blood. They revealed differences in multiple types of immune cells that are involved in the body’s response to COVID-19.
“Using data from three different centres has allowed us to examine how people react to COVID-19,” says John Marioni, Head of Research at EMBL-EBI and Senior Group Leader at the Cancer Research UK Cambridge Institute.
“The amount of data collected in this study has given us crucial insight into the immune reaction in various severities of COVID-19 infection. Analysing single-cell sequencing data requires us to tease apart biological signal from technical noise, which can be very challenging. The work has created a tremendous resource – the most comprehensive blueprint across individuals with different responses to COVID-19.”
Different immune responses
In asymptomatic people, the team found increased levels of B cells that produce antibodies found in mucus passages, such as the nose. These antibodies may be one of our first lines of defence against COVID-19. However, these protective B cells were missing in people with serious symptoms, indicating the importance of an effective antibody-associated immune response in the nose and other mucus passages.
While patients with mild to moderate symptoms had high levels of B cells and helper T-cells, which help to fight infection, the team discovered that those with serious symptoms had lost many of these immune cells, suggesting that this part of the immune system had failed in people with severe disease.
By contrast, people with more serious symptoms leading to hospitalisation had an uncontrolled increase in monocytes and killer T-cells, which can lead to lung inflammation if present at high levels. People with severe disease also had raised levels of platelet-producing cells, which help blood to clot.
Credit: Dr. Zewen Tuong
Potential targets for therapies
These differences in the immune response could help explain serious lung inflammation and blood clotting symptoms, and could be used to identify potential targets for developing therapies.
Professor Menna Clatworthy, senior author and Professor of Translational Immunology at the University of Cambridge and Sanger Associate Faculty, says: “This is one of the most detailed studies of immune responses in COVID-19 to date, and begins to help us understand why some people get really sick while others fight off the virus without even knowing they have it. This new knowledge will help identify specific targets for therapy for patients that get sick with COVID-19.”
John Marioni adds: “This tremendously collaborative project brought together immunologists, medics, and computational biologists in different geographical locations. The work showcases how science is changing and demonstrates that interdisciplinarity is the way forward.”
What is single-cell sequencing?
Single-cell RNA sequencing (scRNA-seq) is a popular and powerful technology that allows researchers to profile the whole transcriptome of a large number of individual cells. The transcriptome of a cell is the collection of RNAs transcribed in it, showing which genes are active.
Single-cell sequencing enables scientists to observe cellular differences at higher resolution, and provides a better understanding of the function of an individual cell in the context of its microenvironment.
Analysis of the large volumes of data generated from these experiments requires specialised statistical and computational methods.
This post was originally published on EMBL-EBI News.