Plasmodium falciparum impairs Ang-1 secretion by pericytes in a 3D brain microvessel model.
EMBO Molecular Medicine 16 October 2025
https://doi.org/10.1038/s44321-025-00319-y
Researchers have built a 3D human blood-brain barrier in the lab and discovered a key role of brain pericytes in cerebral malaria disease
Cerebral malaria is a deadly complication of Plasmodium falciparum infection. Despite cutting-edge research, effective anti-malarial drugs, and the promise of a vaccine, it still claims over half a million lives every year. Many survivors of cerebral malaria suffer long-term disabilities such as epilepsy, speech disorders, or difficulties in movement.
In a new study published in EMBO Molecular Medicine, researchers at EMBL Barcelona highlight malaria-induced disruption of pericytes – cells present along the walls of capillaries – bringing us a step closer to understanding how cerebral malaria damages the brain, and how these damages could be prevented or reversed.
Cerebral malaria infection causes severe damage to the brain’s delicate blood vessels. A central player in this damage is the angiopoietin-Tie signalling pathway, which normally helps blood vessels stay stable, tight, and protected. The normal functioning of this pathway depends on the secretion of a molecule called angiopoietin-1 (Ang-1) by pericytes. Patients with cerebral malaria often show an imbalance in this pathway: too much of the destabilising molecule angiopoietin-2 and too little of the protective Ang-1.
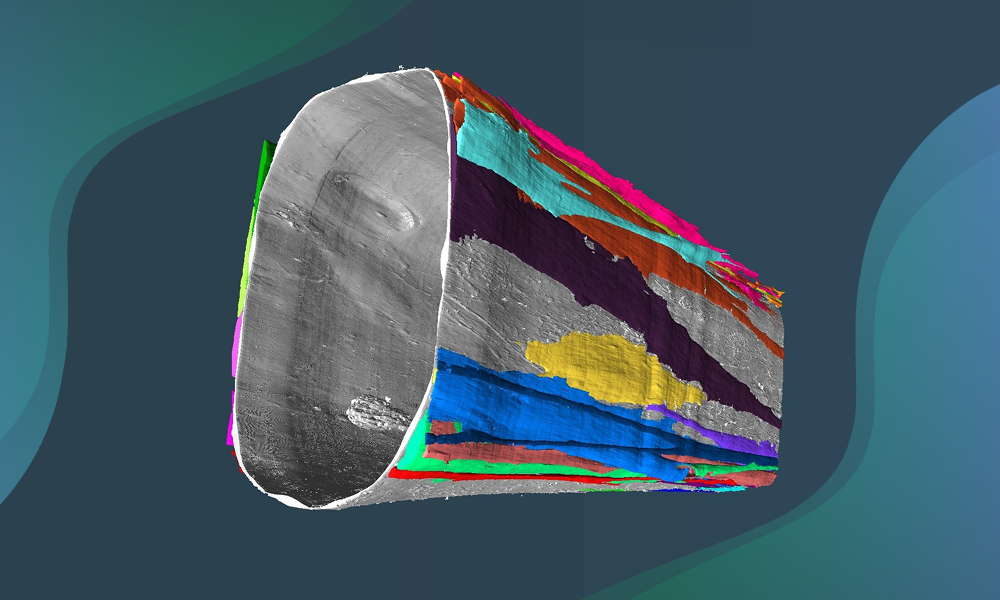
“In this study, we generated an advanced 3D human brain microvasculature model that reproduces important in vivo interactions between human brain endothelial cells and pericytes,” said Rory Long, Postdoctoral Fellow in the Bernabeu Group at EMBL Barcelona and first author of the work. “We show that disruption of the crucial role of pericytes in protecting and restoring the blood vessels promotes blood-brain barrier damage during cerebral malaria.”
The team of researchers built a 3D human blood-brain barrier on a chip and recreated key features of the brain’s vascular (blood-vessel-related) environment. When they exposed this model to malaria parasite byproducts, Ang-1 secretion was halted, vessels became leaky, and the pericytes themselves showed subtle damage. When the researchers added back Ang-1, they were able to partially restore vascular stability, highlighting a connection between decreased Ang-1 secretion and blood-brain barrier breakdown.
To address the urgent need for novel adjunctive treatments against cerebral malaria, the authors then examined the therapeutic potential of the angiopoietin-Tie pathway by using AKB-9778, a drug that boosts Tie-2 activity and is currently in clinical trials for diabetic retinopathy. They found that a short pre-treatment of the 3D blood-brain barrier model with AKB-9778 partially prevented malaria-infected red blood cells from disrupting vasculature integrity. Hence, this study identified AKB-9778 and, more broadly, the restoration of pericyte homeostatic function as an exciting new avenue in cerebral malaria treatment.
“Our bioengineered vascular model is a physiologically relevant platform to test additional therapies for cerebral malaria,” said Maria Bernabeu, EMBL Group Leader and senior author of the publication. “Experimental rodent studies are not ideal for therapeutic discovery, as malaria affects species differently. Our findings pave the way to identify new therapeutics for cerebral malaria patients.”
EMBO Molecular Medicine 16 October 2025
https://doi.org/10.1038/s44321-025-00319-y