Ageing – the intriguing phenomenon of change
 ELLS Guest Blog by Kanchan Anand
ELLS Guest Blog by Kanchan Anand
It is fascinating to learn that a tortoise can easily live over 200 years, while humans rarely cross 100 years. Dogs usually reach the age of 12-15, mice can turn three years of age and mayflies only live a single day. But irrespective of the individual life span, the common denominator remains that eventually all organisms age with time. Ageing affects our tissues and organs like heart, nerves, muscles, bones, and even the brain is no exception. Dementia is one of the age-related brain disorders and Alzheimer’s disease (AD) is one of the most common contributing factors. The year 2010 marked hundred years since the name Alzheimer was coined for AD and, according to some reports (Alzheimer’s disease International, Alzheimer.net), there are already over 36 million cases worldwide – a number which is predicted to triple by the end of 2050. This raises several important questions for scientists, namely how to understand (a) the process of ageing itself and (b) the fundamental basis of age-related disorders such as AD.
While the exact biological cause of ageing still remains to be discovered, the accompanying side effects are being increasingly recognized and researched for. The answers to these questions, in turn, generate another set of questions, namely: do we want to stop ageing, or do we want to merely delay the ageing process, do we prefer to re-generate the degenerated tissues and organs, or are we just satisfied with healthy ageing – free of accompanying disorders such as AD? It is pretty clear that stopping the “age clock” is almost impossible. However, recent research on animal models shows that ageing can be delayed significantly. Attempts towards regenerative therapies have also shown that it is indeed possible to “re-grow” organs and perform organ transplants. Likewise, understanding the biology of AD at a structural level is actively pursued. The aim is to understand how to better age with AD, how to prevent the outbreak of the disease or to develop treatment that allows a normal daily routine.
In order to develop effective therapies to treat AD, one needs to understand in detail the normal, healthy function of the brain as well as the processes underlying this disease. AD is a kind of memory-loss that affects thinking and behavior to the point that it interferes with normal daily routines. It is not part of healthy ageing; however, the risk to develop AD increases with age. Although the majority of people affected by the disease are over 65 years of age, 5% of patients tend to acquire this disease between the age of 40 and 50, with the youngest case reported to be in the late thirties. It is increasingly becoming one of the most common causes of death, especially for older people. On average, patients diagnosed with AD live for a period of about 8 years before they show noticeable symptoms. These facts illustrate the urgent demand for effective treatment of AD.

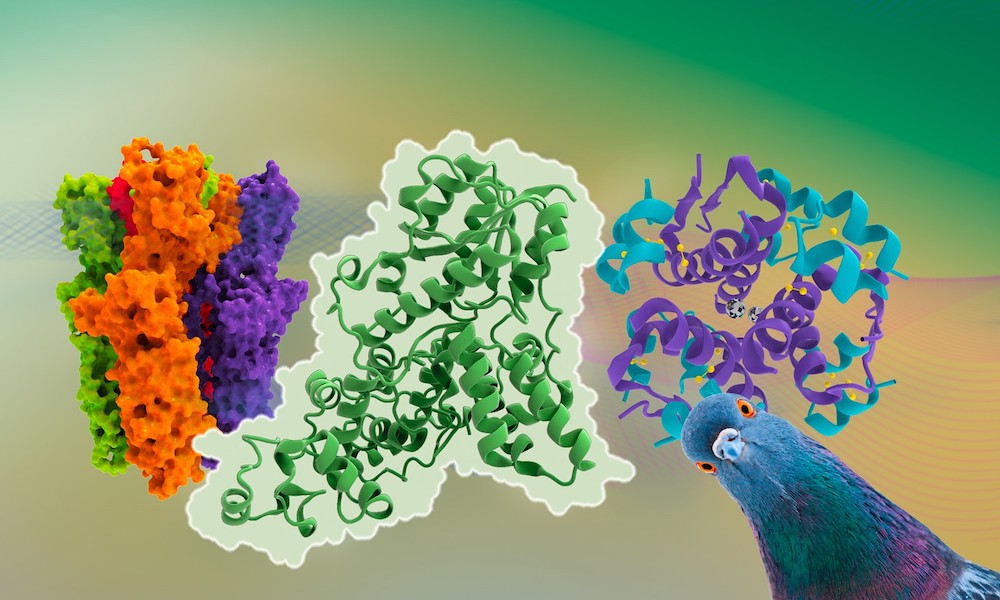
Picture credit: Kanchan Anand
Large scale research efforts are undertaken to investigate the pathology of AD and other related dementias. AD is recognized as a protein mis-folding disease. The three main hypotheses that lead towards the primary cause of AD are known as Cholinergic, Tau and Amyloid hypotheses.
The Cholinergic hypothesis has been known for a long time. It proposes that insufficient production of acetylcholine leads to the disease. Acetylcholine is a neurotransmitter (a brain chemical). Patients with AD seem to produce less acetylcholine, causing loss of memory and cognitive skills over time. All the “first generation medications” were based on this hypothesis and they turn out to only treat the symptoms of the disease to a certain degree but not to cure it. There are a number of medicines on the market today to treat early, middle and severe stages of the disease. The most commonly prescribed class of medicines is called cholinesterase inhibitors (e.g. Donepezil, Rivastigmine and Galantamine). These medicines can help to slowdown the loss of memory. Cholinesterase inhibitors only prevent the breakdown of acetylcholine and they do not trigger the production of acetylcholine. Therefore, they may not be a useful treatment over an extended period of time.
The second hypothesis is based on the tau protein, a microtubule-associated protein expressed in neurons which forms prion-like mis-folded oligomers that eventually lead to AD. Recent studies speculated that a amyloid beta peptide (Aβ 1-42) may induce mis-folding of the ‘tau protein ’resulting in the formation of toxic oligomers
The third well recognized theory is the Amyloid hypothesis. The amyloid beta precursor (APP) is a small membrane associated glycoprotein which gets proteolytically digested to generate a small peptide called Amyloid-beta (Aβ or Abeta), which possesses a central aggregating domain causing this cleaved peptide to aggregate and form toxic oligomers. These aggregated peptides are seen as key causative agents of AD. The normal function of Aβ is not well known but researchers observed its involvement in several functions of the body, e.g. regulation of cholesterol transport, kinase activation, antimicrobial activity and its function as transcription factor. There are several biophysical studies to prove that the central region of Aβ is prone to form β-sheets (hence the name Aβ) which can self-assemble to form a fibrillar structure with poor solubility and high proteolytic stability. This structure is thought to interfere with normal neuronal activity and might thus cause the disease.
How can structural biology help us to turn back the clock on proteins?
To be able to design drugs against any disease, one generally needs to first analyze the structure of the proteins or nucleic acids concerned. In the presented case this is further complicated by additional issues, namely the need to cross the blood-brain barrier to deliver the drug to the brain. Therefore, structural biology can play an important role to understand the organization of complex biological systems. The structure of APP (a multifunctional protein) in complex with different inhibitors has been determined already a decade ago. This structure forms the basis for the presently available drugs. Because of its multifunctional nature, there are several three-dimensional structures of APP that have been solved in order to understand its function and the mechanisms that lead to AD. Using structural biology already in 1999, researchers (J.L.Sussman et al) designed a drug based on the active-site of the Torpedo californica acetylcholinesterase. This drug was finally shown in a complex with human acetylcholinesterase (J.J. Height and his team), which provided precise details for the further development of the drug for humans.
Scientists are looking for new treatments to cure AD and to improve the life of people suffering from AD. Research work published recently in Nature (Nature News doi:10.1038/nature.2014.16291, incl. an animation) has addressed the issue of the blood brain barrier by designing an antibody with two binding sites. One to help with crossing the blood-brain barrier and the second one to disable the enzyme beta-secretase 1 (BACE1) that produces the plaques associated with the disease. One end of the antibody binds loosely to transferrin (a protein that carries iron into the brain) to transport itself into the brain. And once it entered the brain, its other end binds more strongly to BACE1 to stop production of Aβ.
There are more global efforts going on to find better solutions towards therapeutics of this disease, especially towards its prevention, to delay its progression and even to cure it. Researchers are actively unfolding the mysteries underlying the mechanisms of not only AD but also of other age-related disorders that eventually may lead to better treatments and prevention methods. The last decade has shown remarkable progress in this field and we hope that soon we will be able to solve this mystery by better understanding the molecular and cellular processes involved.
Information about the author: The author is a protein x-ray crystallographer. Although her main interest is in viral proteins, she is working on structural aspects of several different proteins that are therapeutic targets.